Strokes are classified into two major types - hemorrhagic and ischemic. Hemorrhagic strokes are due to rupture of a cerebral blood vessel that causes bleeding into or around the brain. Hemorrhagic strokes account for 16% of all strokes. An ischemic stroke is caused by blockage of blood flow in a major cerebral blood vessel, usually due to a blood clot. Ischemic strokes account for about 84% of all strokes. Ischemic strokes are further subdivided based on their etiology into several different categories including thrombotic strokes, embolic strokes, lacunar strokes and hypoperfusion infarctions.
Hemorrhagic strokes account for 16% of all strokes. There are two major categories of hemorrhagic stroke. Intracerebral hemorrhage is the most common, accounting for 10% of all strokes. Subarachnoid hemorrhage, due to rupture of a cerebral aneurysm, accounts for 6% of strokes overall.
The most common cause of non-traumatic intracerebral hematoma is hypertensive hemorrhage. Other causes include amyloid angiopathy, a ruptured vascular malformation, coagulopathy, hemorrhage into a tumor, venous infarction, and drug abuse.
Hypertensive hemorrhage accounts for approximately 70-90% of non-traumatic primary intracerebral hemorrhages. It is commonly due to vasculopathy involving deep penetrating arteries of the brain. Hypertensive hemorrhage has a predilection for deep structures including the thalamus, pons, cerebellum, and basal ganglia, particularly the putamen and external capsule. Thus, it often appears as a high-density hemorrhage in the region of the basal ganglia. Blood may extend into the ventricular system. Intraventricular extension of the hematoma is associated with a poor prognosis.
Coagulopathy Related Intracerebral Hemorrhage
Coagulopathy related intracerebral hemorrhage can be due to drugs such as coumadin or a systemic abnormality such as thrombocytopenia. On imaging, this hemorrhage often has a heterogeneous appearance due to incompletely clotted blood. A fluid level within a hematoma suggest coagulopathy as an underlying mechanism.
Hemorrhage Due to Arteriovenous Malformation
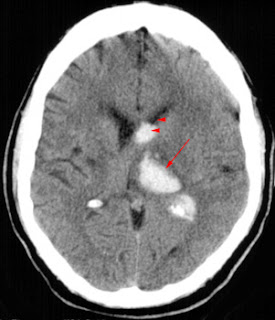
An underlying arteriovenous malformation (AVM) may or may not be visible on a CT scan. However, prominent vessels adjacent to the hematoma suggest an underlying arteriovenous malformation. In addition, some arteriovenous malformations contain dysplastic areas of calcification and may be visible as serpentine enhancing structures after contrast administration.

 The CT on the above shows hemorrhage (arrow) due to underlying AVM (arrowheads). The arteriogram on the down shows the tangle of vessels (arrowheads) of the AVM. This lesion would be considered for intravascular embolic therapy.
The CT on the above shows hemorrhage (arrow) due to underlying AVM (arrowheads). The arteriogram on the down shows the tangle of vessels (arrowheads) of the AVM. This lesion would be considered for intravascular embolic therapy.Subarachnoid Hemorrhage
In the absence of trauma, the most common cause of subarachnoid hemorrhage is a ruptured cerebral aneurysm. Cerebral aneurysms tend to occur at branch points of intracranial vessels and thus are frequently located around the Circle of Willis. Common aneurysm locations include the anterior and posterior communicating arteries, the middle cerebral artery bifurcation and the tip of the basilar artery. Subarachnoid hemorrhage typically presents as the "worst headache of life" for the patient. Detection of a subarachnoid hemorrhage is crucial because the rehemorrhage rate of ruptured aneurysms is high and rehemorrhage is often fatal.CT is currently the imaging modality of choice because of its high sensitivity for the detection of subarachnoid hemorrhage. CT is most sensitive for acute subarachnoid hemorrhage. After a period of days to weeks CT becomes much less sensitive as blood is resorbed from the CSF. If there is a strong clinical indication, LP may be warranted despite a negative CT since small bleeds can be unapparent on imaging.On CT, a subarachnoid hemorrhage appears as high density within sulci and cisterns. The insular regions and basilar cisterns should be carefully scrutinized for subtle signs of subarachnoid hemorrhage. Subarachnoid hemorrhage may have associated intraventricular hemorrhage and hydrocephalus.
 High density blood fills the cisterns (arrowheads) in this patient with hemorrhage from the left middle cerebral artery. Note the middle cerebral artery aneurysm (arrows).
High density blood fills the cisterns (arrowheads) in this patient with hemorrhage from the left middle cerebral artery. Note the middle cerebral artery aneurysm (arrows). Ischemic stroke
Ischemic strokes are caused by thrombosis, embolism of thrombosis, hypoperfusion and lacunar infarctions. A thrombotic stroke occurs when a blood clot forms in situ within a cerebral artery and blocks or reduces the flow of blood through the artery. This may be due to an underlying stenosis, rupture of an atherosclerotic plaque, hemorrhage within the wall of the blood vessel, or an underlying hypercoagulable state. This may be preceded by a transient ischemic attack and often occurs at night or in the morning when blood pressure is low. Thrombotic ischemic strokes account for 53% of all strokes.An embolic stroke occurs when a detached clot flows into and blocks a cerebral artery. The detached clot often originates from the heart or from the walls of large vessels such as the carotid arteries. Atrial fibrillation is also a common cause. Embolic strokes account for 30% of all strokes.A lacunar infarction occurs when the walls of small arteries thicken and cause the occlusion of the artery. These typically involve the small perforating vessels of the brain and result in lesions that are less than 1.5 cm in size.Hypoperfusion infarctions occur under two circumstances. Global anoxia may occur from cardiac or respiratory failure and presents an ischemic challenge to the brain. Tissue downstream from a severe proximal stenosis of a cerebral artery may undergo a localized hypoperfusion infarction. Lacunar and hypoperfusion strokes, account for the remaining 1% of strokes of the ischemic type.
Imaging of Stroke
"Stroke" is a clinical diagnosis; however imaging is playing an increasingly important role in its diagnosis and management. The most important issue to determine when imaging a stroke patient is whether one is dealing with a hemorrhagic or ischemic event. This has crucial therapeutic and triage implications. Decisions that must be made concerning therapy are dependent on the diagnosis and may include the following:- Is the patient a thrombolysis candidate and should thrombolytic therapy be used?- Intravenous or intrarterial therapy?- Neurosurgery or neurology patient?In addition about 2% of clinically definite "strokes" are found to be a result of some other pathology such as a tumor, a subdural hematoma or an infection.
CT scanning
There are several advantages to performing a CT scan instead of other imaging modalities. A CT scan:- Is readily available- Is rapid- Allows easy exclusion of hemorrhage- Allows the assessment of parenchymal damageThe disadvantages of CT include the following:- Old versus new infarcts is not always clear- No functional information (yet)- Limited evaluation of vertebrobasilar systemA CT is 58% sensitive for infarction within the first 24 hours (Bryan et al, 1991). MRI is 82% sensitive. If the patient is imaged greater than 24 hours after the event, both CT and MR are greater than 90% sensitive.
CT Pathophysiology
After a stroke, edema progresses, and brain density decreases proportionately. Severe ischemia results in a 3% increase in intraparenchymal water within 1 hour. This corresponds to 7-8 Hounsfield Unit decrease in brain density. There is also a 6% increase in water at 6 hours. The degree of edema is related to the severity of hypoperfusion and the adequacy of collateral vessels.
 Sharply circumscribed hypodense edema (arrowheads) in the right middle cerebral artery territory.
Sharply circumscribed hypodense edema (arrowheads) in the right middle cerebral artery territory.CT Findings of Stroke
When analyzing the CT of a potential stroke victim, one of the first findings to look for is the presence or absence of hemorrhage. Another common finding in stroke patients is a dense middle cerebral artery or a dense basilar artery, which corresponds to thrombus in the affected vessel. There are also more subtle changes of acute ischemia due to edema which include the following:- Obscuration of the lentiform nuclei- Loss of insular ribbon- Loss of gray/white distinction- Sulcal effacement
 Dense basilar artery (arrow).
Dense basilar artery (arrow).Hyperdense Vessel Sign
 High density in the right middle cerebral artery (arrowheads).Compare it with the normal left middle cerebral artery (arrow).
High density in the right middle cerebral artery (arrowheads).Compare it with the normal left middle cerebral artery (arrow).Thrombosis of the basilar artery is a common finding in stroke patients. CT findings include a dense basilar artery without contrast injection.
 Dense basilar artery (arrow). Compare this to the normal internal carotid artery (arrowhead).
Dense basilar artery (arrow). Compare this to the normal internal carotid artery (arrowhead).Lentiform nucleus obscuration is due to cytotoxic edema in the basal ganglia. This sign indicates proximal middle cerebral artery occlusion, which results in limited flow to lenticulostriate arteries. Lentiform nucleus obscuration can be seen as early as one hour post onset of stroke.
 Hypodensity in the left hemisphere (arrows) involving the caudate nucleus and lentiform nuclei (globus pallidus and putamen).
Hypodensity in the left hemisphere (arrows) involving the caudate nucleus and lentiform nuclei (globus pallidus and putamen).The insular ribbon sign is the loss of the gray-white interface in the lateral margins of the insula. This area is supplied by the insular segment of the middle cerebral artery and is particularly susceptible to ischemia because it is the most distal region from either anterior or posterior collaterals. The insular ribbon sign may involve only the anterior or the posterior insula.
 The cortex of the left insular ribbon is not visualized (arrow).
The cortex of the left insular ribbon is not visualized (arrow).Diffuse hypodensity and sulcal effacement is the most consistent sign of infarction. Extensive parenchymal hypodensity is associated with poor outcome. If this sign is present in greater than 50% of the middle cerebral artery territory there is, on average, an 85% mortality rate. Hypodensity in greater than one-third of the middle cerebral artery territory is generally considered to be a contra-indication to thrombolytic therapy.
 Hypodensity and sulcal effacement (arrowheads)in the right middle cerebral artery distribution.
Hypodensity and sulcal effacement (arrowheads)in the right middle cerebral artery distribution.The CT of a subactue infarction has the following findings in 1 -3 days:- Increasing mass effect- Wedge shaped low density- Hemorrhagic transformationAfter 4 - 7 days the CT is characterized by:- Gyral enhancement- Persistent mass effectIn 1-8 weeks:- Mass effect resolves- Enhancement may persist
 This image was taken 4 hours after the infarction.
This image was taken 4 hours after the infarction. This image, from the same patient, was taken 2 days after the infaction.
This image, from the same patient, was taken 2 days after the infaction.
Enhancement in Infarctions
Ninety percent of infarcts enhance on CT examinations with intravenous contrast at 1 week after the infarct. Approximately 35% enhance by 3 days. Faint enhancement begins near the pial surface or near the infarct margins. The enhancement is initially smaller than the area of infarction. It subsequently becomes gyriform. Enhancement is due to breakdown of the blood brain barrier, neovascularity, and reperfusion of damaged brain tissue. Post contrast CT scan demonstrating gyriform enhancementof subacute right frontal lobe infarct (arrow).
Post contrast CT scan demonstrating gyriform enhancementof subacute right frontal lobe infarct (arrow).
Reference:University of Virginia Health Sciences Center, Department of Radiology website.






NICE.. HEAVY WORK UP..
ReplyDelete