ESSENTIALS
-Many patients with inflammatory or infectious types of colitis present with abdominal pain, and multidetector CT is often used as the initial diagnostic test.
-CT can accurately depict the bowel wall and help determine the presence and extent of intramural disease, its possible extraluminal extension, and involvement of distant sites.
-Many imaging features or patterns are helpful in distinguishing the various types of colitis, including degree of wall thickening, extent and location of disease, extraluminal manifestations, and types of complication.
-While imaging features can help narrow the differential diagnosis or suggest a specific diagnosis, the final diagnosis is often based on clinical and laboratory data and colonoscopic and biopsy findings.
radiology.rsna.org/content/240/3/623.full
Saturday, June 12, 2010
 Transverse CT image in a 67-year-old woman with acute right upper quadrant pain due to omental infarction shows ill-defined, ovoid, fatty mass (arrows) of increased attenuation centered in the greater omentum.
Transverse CT image in a 67-year-old woman with acute right upper quadrant pain due to omental infarction shows ill-defined, ovoid, fatty mass (arrows) of increased attenuation centered in the greater omentum.radiology.rsna.org/content/240/3/623.full
 Transverse CT image in a 34-year-old man with acute right lower quadrant pain caused by appendicitis with perforation. Appendiceal lumen (short black arrow) is enlarged and shows wall enhancement. Mesenteric stranding (white arrow), free intraperitoneal air (arrowhead), and thickened terminal ileum (long black arrow) due to contiguous inflammation are seen.
Transverse CT image in a 34-year-old man with acute right lower quadrant pain caused by appendicitis with perforation. Appendiceal lumen (short black arrow) is enlarged and shows wall enhancement. Mesenteric stranding (white arrow), free intraperitoneal air (arrowhead), and thickened terminal ileum (long black arrow) due to contiguous inflammation are seen.radiology.rsna.org/content/240/3/623.full
 Transverse CT image in a 21-year-old man with right lower quadrant pain due to appendicitis shows an appendicolith (arrowhead) separated from cecal lumen by cecal wall thickening (cecal bar sign) (black arrow). Dilatation of inflamed appendix with air and debris (white arrow) is demonstrated.
Transverse CT image in a 21-year-old man with right lower quadrant pain due to appendicitis shows an appendicolith (arrowhead) separated from cecal lumen by cecal wall thickening (cecal bar sign) (black arrow). Dilatation of inflamed appendix with air and debris (white arrow) is demonstrated.radiology.rsna.org/content/240/3/623.full

Transverse CT image in a 65-year-old woman with early diverticulitis who had left lower quadrant pain and leukocytosis reveals wall thickening and multiple small diverticula (arrows) in a long segment of the sigmoid colon. Fascial thickening (arrowheads) along left pelvic side wall indicates mild diverticulitis.
 a
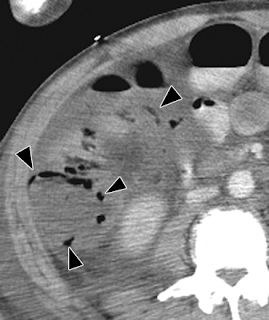
aIschemic colitis in an 81-year-old woman with myocardial infarction. (a) Anteroposterior CT scout view shows air (arrows) in wall of right colon and small- and large-bowel dilatation. (b) Transverse CT image demonstrates air (arrowheads) in wall of right colon, with lack of wall enhancement and pericolonic stranding indicative of infarction.
 Transverse CT image in a 22-year-old woman with ischemic colitis after blunt abdominal trauma to right flank demonstrates marked thickening of hepatic flexure and right colon, with abrupt transition (arrows) between abnormal and normal wall in the transverse colon.
Transverse CT image in a 22-year-old woman with ischemic colitis after blunt abdominal trauma to right flank demonstrates marked thickening of hepatic flexure and right colon, with abrupt transition (arrows) between abnormal and normal wall in the transverse colon.radiology.rsna.org/content/240/3/623.full
 Transverse CT image in a 71-year-old man with ischemic colitis due to arrhythmia shows ascites and marked thickening of sigmoid colon associated with multiple large nodular defects, which are the CT analog of thumbprinting (arrows) on radiographs. Note that rectal wall (arrowheads) is normal.
Transverse CT image in a 71-year-old man with ischemic colitis due to arrhythmia shows ascites and marked thickening of sigmoid colon associated with multiple large nodular defects, which are the CT analog of thumbprinting (arrows) on radiographs. Note that rectal wall (arrowheads) is normal.radiology.rsna.org/content/240/3/623.full
 Transverse CT image in a 45-year-old male transplantation patient with neutropenic colitis shows marked wall thickening in ascending colon (arrow) associated with pericolonic stranding and ascites (arrowheads).
Transverse CT image in a 45-year-old male transplantation patient with neutropenic colitis shows marked wall thickening in ascending colon (arrow) associated with pericolonic stranding and ascites (arrowheads).radiology.rsna.org/content/240/3/623.full
 Transverse CT image in a 9-year-old girl with myelogenous leukemia and typhlitis demonstrates marked wall thickening in cecum (arrow) and terminal ileum (arrowhead).
Transverse CT image in a 9-year-old girl with myelogenous leukemia and typhlitis demonstrates marked wall thickening in cecum (arrow) and terminal ileum (arrowhead).radiology.rsna.org/content/240/3/623.full
 a
aTransverse CT images in a 31-year-old man with amebiasis who had a history of diarrhea and recent travel to North Africa. (a) Cecal wall is thickened (arrow), but terminal ileum (arrowheads) is not involved. (b) Hepatic flexure (arrows) also demonstrates marked thickening, but descending colon (arrowhead) appears normal.
 Transverse CT image in a 60-year-old man with fistula formation due to tuberculous colitis. Descending colon appears slightly thickened, and a fistulous tract (white arrows) is shown to extend from the colon to an abscess (black arrow) in the left psoas muscle and through the left paraspinal muscles into the subcutaneous tissue of the back, where another abscess (arrowheads) has formed.
Transverse CT image in a 60-year-old man with fistula formation due to tuberculous colitis. Descending colon appears slightly thickened, and a fistulous tract (white arrows) is shown to extend from the colon to an abscess (black arrow) in the left psoas muscle and through the left paraspinal muscles into the subcutaneous tissue of the back, where another abscess (arrowheads) has formed.radiology.rsna.org/content/240/3/623.full
 Transverse CT image in a 33-year-old man with tuberculous ileocolitis who had recently emigrated from Southeast Asia. The cecal wall (arrows) and terminal ileum (arrowheads) are markedly thickened.
Transverse CT image in a 33-year-old man with tuberculous ileocolitis who had recently emigrated from Southeast Asia. The cecal wall (arrows) and terminal ileum (arrowheads) are markedly thickened.radiology.rsna.org/content/240/3/623.full

 CT images in a 37-year-old woman with Crohn disease (ileocolitis). (a) Transverse scan obtained following enteroclysis demonstrates ileoileal (arrow) and ileosigmoidal fistulae (arrowhead). The involved ileal and colonic wall is asymmetrically thickened. (b) Coronal reformation shows ileoileal fistula (arrow) quite well. Contrast enhancement in vagina (arrowheads) is due to an ileovaginal fistula. (Images courtesy of John Lappas, MD, University of Indiana.)
CT images in a 37-year-old woman with Crohn disease (ileocolitis). (a) Transverse scan obtained following enteroclysis demonstrates ileoileal (arrow) and ileosigmoidal fistulae (arrowhead). The involved ileal and colonic wall is asymmetrically thickened. (b) Coronal reformation shows ileoileal fistula (arrow) quite well. Contrast enhancement in vagina (arrowheads) is due to an ileovaginal fistula. (Images courtesy of John Lappas, MD, University of Indiana.)  Transverse CT image in a 35-year-old patient with ulcerative colitis and toxic megacolon shows markedly distended transverse colon with shaggy mucosa (arrows).
Transverse CT image in a 35-year-old patient with ulcerative colitis and toxic megacolon shows markedly distended transverse colon with shaggy mucosa (arrows).radiology.rsna.org/content/240/3/623.full
 Transverse CT image in a 24-year-old woman with Crohn ileocolitis shows thickening of terminal ileum and cecum (white arrows) with fibrofatty proliferation (arrowheads) in right lower quadrant. One enlarged lymph node (black arrow) is also depicted.
Transverse CT image in a 24-year-old woman with Crohn ileocolitis shows thickening of terminal ileum and cecum (white arrows) with fibrofatty proliferation (arrowheads) in right lower quadrant. One enlarged lymph node (black arrow) is also depicted.radiology.rsna.org/content/240/3/623.full
 Transverse CT image in a 32-year-old woman with ulcerative colitis and bloody diarrhea demonstrates the double halo, or target, sign with inner (mucosa, arrow) and outer (muscularis propria, arrowhead) rings of high attenuation separated by a ring of low attenuation, which represents submucosa with edema. Little if any pericolonic stranding is seen.
Transverse CT image in a 32-year-old woman with ulcerative colitis and bloody diarrhea demonstrates the double halo, or target, sign with inner (mucosa, arrow) and outer (muscularis propria, arrowhead) rings of high attenuation separated by a ring of low attenuation, which represents submucosa with edema. Little if any pericolonic stranding is seen.http://www.google.com.eg/imgres?imgurl=http://radiology.rsna.org/content/240/3/623/F16.small.gif&imgrefurl=http://radiology.rsna.org/content/240/3/623.full&usg=__TEFfqDAl8UDupdZnziMD_QJcGvU=&h=187&w=200&sz=34&hl=en&start=25&itbs=1&tbnid=0LErWAgkUG2ioM:&tbnh=97&tbnw=104&prev=/images%3Fq%3Dleukaemia%2Bradiology%26start%3D20%26hl%3Den%26sa%3DN%26gbv%3D2%26ndsp%3D20%26tbs%3Disch:1
 Distinction between Ulcerative Colitis and Crohn Disease
Distinction between Ulcerative Colitis and Crohn Diseasehttp://www.google.com.eg/imgres?imgurl=http://radiology.rsna.org/content/240/3/623/F16.small.gif&imgrefurl=http://radiology.rsna.org/content/240/3/623.full&usg=__TEFfqDAl8UDupdZnziMD_QJcGvU=&h=187&w=200&sz=34&hl=en&start=25&itbs=1&tbnid=0LErWAgkUG2ioM:&tbnh=97&tbnw=104&prev=/images%3Fq%3Dleukaemia%2Bradiology%26start%3D20%26hl%3Den%26sa%3DN%26gbv%3D2%26ndsp%3D20%26tbs%3Disch:1
 Transverse CT image in a 45-year-old man with chronic ulcerative colitis. Thickened rectal wall demonstrates the fat halo sign (arrowhead). Perirectal fat (arrows) is increased.
Transverse CT image in a 45-year-old man with chronic ulcerative colitis. Thickened rectal wall demonstrates the fat halo sign (arrowhead). Perirectal fat (arrows) is increased.http://www.google.com.eg/imgres?imgurl=http://radiology.rsna.org/content/240/3/623/F16.small.gif&imgrefurl=http://radiology.rsna.org/content/240/3/623.full&usg=__TEFfqDAl8UDupdZnziMD_QJcGvU=&h=187&w=200&sz=34&hl=en&start=25&itbs=1&tbnid=0LErWAgkUG2ioM:&tbnh=97&tbnw=104&prev=/images%3Fq%3Dleukaemia%2Bradiology%26start%3D20%26hl%3Den%26sa%3DN%26gbv%3D2%26ndsp%3D20%26tbs%3Disch:1
 Transverse CT image in a 39-year-old man with Crohn disease (granulomatous ileocolitis) shows thickening of the ileocecal tip (arrows) and marked thickening of the terminal ileum (arrowheads). The ileocecal valve is stenosed, as demonstrated by succus in the lumen and prestenotic dilatation.
Transverse CT image in a 39-year-old man with Crohn disease (granulomatous ileocolitis) shows thickening of the ileocecal tip (arrows) and marked thickening of the terminal ileum (arrowheads). The ileocecal valve is stenosed, as demonstrated by succus in the lumen and prestenotic dilatation.http://www.google.com.eg/imgres?imgurl=http://radiology.rsna.org/content/240/3/623/F16.small.gif&imgrefurl=http://radiology.rsna.org/content/240/3/623.full&usg=__TEFfqDAl8UDupdZnziMD_QJcGvU=&h=187&w=200&sz=34&hl=en&start=25&itbs=1&tbnid=0LErWAgkUG2ioM:&tbnh=97&tbnw=104&prev=/images%3Fq%3Dleukaemia%2Bradiology%26start%3D20%26hl%3Den%26sa%3DN%26gbv%3D2%26ndsp%3D20%26tbs%3Disch:1
 Transverse CT image in a 34-year-old woman with ulcerative colitis. The wall of the sigmoid is thickened, and hyperemic mesenteric arteries (arrowheads) appear as bright dots next to the outer wall of the colon. This indicates active disease.
Transverse CT image in a 34-year-old woman with ulcerative colitis. The wall of the sigmoid is thickened, and hyperemic mesenteric arteries (arrowheads) appear as bright dots next to the outer wall of the colon. This indicates active disease.http://www.google.com.eg/imgres?imgurl=http://radiology.rsna.org/content/240/3/623/F16.small.gif&imgrefurl=http://radiology.rsna.org/content/240/3/623.full&usg=__TEFfqDAl8UDupdZnziMD_QJcGvU=&h=187&w=200&sz=34&hl=en&start=25&itbs=1&tbnid=0LErWAgkUG2ioM:&tbnh=97&tbnw=104&prev=/images%3Fq%3Dleukaemia%2Bradiology%26start%3D20%26hl%3Den%26sa%3DN%26gbv%3D2%26ndsp%3D20%26tbs%3Disch:1
 Transverse CT image of normal rectosigmoid colon in a 45-year-old man. The wall of the rectosigmoid colon (arrows) is enhanced, and the colon is well distended with water.
Transverse CT image of normal rectosigmoid colon in a 45-year-old man. The wall of the rectosigmoid colon (arrows) is enhanced, and the colon is well distended with water.http://www.google.com.eg/imgres?imgurl=http://radiology.rsna.org/content/240/3/623/F16.small.gif&imgrefurl=http://radiology.rsna.org/content/240/3/623.full&usg=__TEFfqDAl8UDupdZnziMD_QJcGvU=&h=187&w=200&sz=34&hl=en&start=25&itbs=1&tbnid=0LErWAgkUG2ioM:&tbnh=97&tbnw=104&prev=/images%3Fq%3Dleukaemia%2Bradiology%26start%3D20%26hl%3Den%26sa%3DN%26gbv%3D2%26ndsp%3D20%26tbs%3Disch:1
Friday, June 11, 2010
 a
aHistologically proved yolk sac tumor in a 1-year-old boy with a painless unilateral scrotal mass. (a) Longitudinal US scan of the left hemiscrotum shows a solid tumor (T) replacing the entire testis. The cystic areas (arrowheads) represent tumor necrosis. (b) Contrast-enhanced abdominal CT scan, obtained during the initial work-up, shows retroperitoneal lymphadenopathy (L) with necrotic areas.
 Epididymal cyst in a boy with a palpable scrotal mass. Longitudinal US scan shows a cystic lesion (C) that demonstrates increased sound transmission and replaces almost the entire epididymal head. This US appearance is indistinguishable from that of a spermatocele. T = testis.
Epididymal cyst in a boy with a palpable scrotal mass. Longitudinal US scan shows a cystic lesion (C) that demonstrates increased sound transmission and replaces almost the entire epididymal head. This US appearance is indistinguishable from that of a spermatocele. T = testis.http://radiographics.rsna.org/content/25/5/1197.figures-only
 A
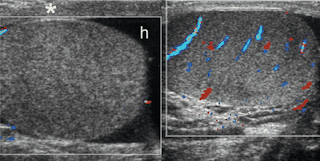
ATesticular torsion in a 12-year-old boy with right-sided scrotal pain of sudden onset. (a) Longitudinal US scan of the right hemiscrotum shows a round supratesticular mass (M), which represents an edematous spermatic cord. There are several anechoic structures (arrowheads) within the mass, which probably represent obstructed and dilated lymphatic vessels. T = testis. (b) Bilateral transverse color Doppler images show no color flow signals in the right testis, which is enlarged and has heterogeneous echogenicity. Reactive hydrocele (h) and thickening of the scrotal wall (*) are also seen. Testicular torsion and bell clapper deformity were confirmed at surgery.
 A
A B
BNormal and twisted testicular appendages. (a) Longitudinal power Doppler image of a 10-year-old boy with a hydrocele shows the normal appendix testis as a round structure (arrow) that is isoechoic relative to the testis and is supplied by a branch of the capsular artery. (b) Longitudinal US scan of the left hemiscrotum in a patient with scrotal pain and swelling shows a highly echogenic well-defined mass (arrows) at the upper pole of the epididymis (E). The mass represents a twisted epididymal appendage. T = testis. (c) Color Doppler image of the same patient shows that the twisted appendage is avascular (arrows). Mild reactive hypervascularity is seen at the epididymal head and scrotal tunics.
 Acute epididymitis in a 9-year-old boy with scrotal pain and redness. Longitudinal US scan shows that the epididymal head and body (arrows) are enlarged and hypoechoic relative to the normal testis (T). Wall thickening (*) and reactive hydrocele (h) are also seen. Power Doppler imaging showed increased perfusion of the epididymis.
Acute epididymitis in a 9-year-old boy with scrotal pain and redness. Longitudinal US scan shows that the epididymal head and body (arrows) are enlarged and hypoechoic relative to the normal testis (T). Wall thickening (*) and reactive hydrocele (h) are also seen. Power Doppler imaging showed increased perfusion of the epididymis.http://radiographics.rsna.org/content/25/5/1197.figures-only
 A
AClinically proved epididymitis in an 11-year-old boy. (a) Longitudinal US scan of the right hemiscrotum shows an enlarged hypoechoic epididymal head (E), reactive hydrocele (h), and thickening of the scrotal wall (*). m = mediastinum. (b) Color and pulsed-wave Doppler image shows increased vascularity in the epididymal head with a low-flow, low-resistance waveform pattern.


 Left varicocele in a 15-year-old boy. (a) Longitudinal US scan of the left hemiscrotum shows multiple anechoic structures (arrows) in the supratesticular region and extending behind the upper pole of the testis (T). (b) Color Doppler image shows that the anechoic structures are vascular. (c) Pulsed-wave Doppler image shows a venous waveform with increased flow during the Valsalva maneuver (arrow).
Left varicocele in a 15-year-old boy. (a) Longitudinal US scan of the left hemiscrotum shows multiple anechoic structures (arrows) in the supratesticular region and extending behind the upper pole of the testis (T). (b) Color Doppler image shows that the anechoic structures are vascular. (c) Pulsed-wave Doppler image shows a venous waveform with increased flow during the Valsalva maneuver (arrow).  It is not uncommon to see two or three tiny calcifications in the testicle. Mutiple tiny calcifications throughout the testes have been found and are termed microlithiasis. Although microlithiasis has been seen in normal patients, it is associated with tumors, sterility, and cryptorchidism. Sonographically, microlithiasis appears as multiple echogenic non-shadowing areas throughout the testis, and these calcifications may obscure other pathologic conditions.
It is not uncommon to see two or three tiny calcifications in the testicle. Mutiple tiny calcifications throughout the testes have been found and are termed microlithiasis. Although microlithiasis has been seen in normal patients, it is associated with tumors, sterility, and cryptorchidism. Sonographically, microlithiasis appears as multiple echogenic non-shadowing areas throughout the testis, and these calcifications may obscure other pathologic conditions.http://www.blogger.com/www.gehealthcare.com/.../cme_scrotal.html
A varicocele is the abnormal dilation and tortuosity of the veins in the pampiniform plexus that run along the spermatic cord into the scrotum. The spermatic cord provides nourishment through the blood vessels and contains nerves and lymph glands as well as the vas deferens. Varicoceles are reported to be found in 15% of all males. They are found to be the cause of infertility in 30-40% of the cases. The varicoceles develop when a defective valve in the vein allows the normal one-way flow of blood to back up into the abdomen. Blood then flows from the abdomen into the scrotum where a hostile environment for sperm development is created. Most varicoceles develop slowly and do not show symptoms. Some are large and visible as twisting veins in the scrotal sac. These veins disappear when lying down and the valsalva maneuver (bear down or cough) is used to demonstrated their filling distention.
They are more common on the left side, but do also occur bilaterally. The right internal spermatic vein drains directly into the inferior vena cava, whereas the left internal spermatic vein drains into the left renal vein at a 90-degree angle. This angle prevents the formation of a valve. As a result, 85-99% of the varicoceles are left-sided and only 1% are bilateral.
Varicoceles may cause infertility because they are associated with low sperm counts and decreased mobility. Sonographically they appear as an extratesticular collection of tortuous tubular structures.
http://www.blogger.com/www.gehealthcare.com/.../cme_scrotal.html
They are more common on the left side, but do also occur bilaterally. The right internal spermatic vein drains directly into the inferior vena cava, whereas the left internal spermatic vein drains into the left renal vein at a 90-degree angle. This angle prevents the formation of a valve. As a result, 85-99% of the varicoceles are left-sided and only 1% are bilateral.
Varicoceles may cause infertility because they are associated with low sperm counts and decreased mobility. Sonographically they appear as an extratesticular collection of tortuous tubular structures.
http://www.blogger.com/www.gehealthcare.com/.../cme_scrotal.html
 A hydrocele is a collection of fluid between the visceral and parietal layers of the tunica vaginalis. Hydroceles can be congenital, idiopathic, or acquired. Acquired hydroceles are the results of infarction, inflammation, neoplasm, or trauma.
A hydrocele is a collection of fluid between the visceral and parietal layers of the tunica vaginalis. Hydroceles can be congenital, idiopathic, or acquired. Acquired hydroceles are the results of infarction, inflammation, neoplasm, or trauma.Sonographically hydroceles may appears as anechoic fluid in the scrotal sac surrounding the testicle and epididymis. Occasionally, small particles and septations are seen within the fluid.
http://www.blogger.com/www.gehealthcare.com/.../cme_scrotal.html

Spermatoceles. A spermatocele is a benign cyst consisting of nonviable sperm. They are commonly located in the head of the epididymis, but have been found in the body and tail as well. Septations have been seen with the cysts. The spermatoceles may be singular or multiple
On sonography, a spermatocele appears as a cyst, anechoic with posterior enhancement with rounded, well-defined walls. A spermatocele cannot be differentiated from a simple epididymal cyst.
Epididymal Cysts. These masses are composed of clear serous fluid, not sperm and are much less common than spermatoceles. Sonographically they present as a typical cystic type appearance with well-defined walls and good transmission.
http://www.blogger.com/www.gehealthcare.com/.../cme_scrotal.html
On sonography, a spermatocele appears as a cyst, anechoic with posterior enhancement with rounded, well-defined walls. A spermatocele cannot be differentiated from a simple epididymal cyst.
Epididymal Cysts. These masses are composed of clear serous fluid, not sperm and are much less common than spermatoceles. Sonographically they present as a typical cystic type appearance with well-defined walls and good transmission.
http://www.blogger.com/www.gehealthcare.com/.../cme_scrotal.html
 Sonographically, a torsed testicle appears normal in the first four hours of torsion. Although the realtime appearance of the testes is normal, Color and pulsed-Doppler appearances are abnormal. There is an absence of flow in the testicle and the epididymis. After four hours, the torsed testicle appears enlarged and hypoechoic. The testicle may have some inhomogenous appearances as a result of hemorrhage. Other findings include enlargement of the epidiymis, a reactive hydrocele, and scrotal wall thickening.
Sonographically, a torsed testicle appears normal in the first four hours of torsion. Although the realtime appearance of the testes is normal, Color and pulsed-Doppler appearances are abnormal. There is an absence of flow in the testicle and the epididymis. After four hours, the torsed testicle appears enlarged and hypoechoic. The testicle may have some inhomogenous appearances as a result of hemorrhage. Other findings include enlargement of the epidiymis, a reactive hydrocele, and scrotal wall thickening.http://www.blogger.com/www.gehealthcare.com/.../cme_scrotal.html
Trauma. A direct blow to the scrotal sac can cause significant testicular parenchymal injury or hemorrhage and can definitely alter the normal homogeneous appearance of the testicle. Hematomas in the epididymis or scrotal wall may have variable sonographic appearances. Just like hematomas in other parts of the body, their appearance may vary depending upon the age of the hematoma. At first the hematoma will be hypoechoic as the red blood cells fill the space; as the hematoma ages, its appearance becomes more echogenic as clot begins to form within the bleed.
http://www.blogger.com/www.gehealthcare.com/.../cme_scrotal.html
http://www.blogger.com/www.gehealthcare.com/.../cme_scrotal.html

Orchitis. Once the infection has spread to the testicle, it is termed orchitis. The testicle may appear normal or enlarged in size and the echogenicity may be decreased or heterogeneous. Reactive hydroceles and skin thickening are associated with orchitis. As in many infections, there will be increased color Dopplor flow to the infected testes. Chronic orchitis appears as layers of heterogeneous disruption within the testicle. Focal orchitis may occur without involvement of the epididymis and has the same appearance as a neoplasm, although clinical symptoms such as fever and increased white blood cell count strongly would suggest an infectious process.
http://www.google.com.eg/imgres?imgurl=http://www.gehealthcare.com/usen/ultrasound/images/cme_scrotal5_500.jpg&imgrefurl=http://www.gehealthcare.com/usen/ultrasound/products/cme_scrotal.html&usg=__pRNzx5ouiF10cwNwsoFkjfJSRXA=&h=500&w=500&sz=36&hl=en&start=3&sig2=ks6xO2TYTwxfQlNMvO1feQ&itbs=1&tbnid=OE4rpucS1ksjsM:&tbnh=130&tbnw=130&prev=/images%3Fq%3Dscrotal%2Bultrasound%26hl%3Den%26gbv%3D2%26tbs%3Disch:1&ei=HV8STNq1HdCg4QbzxKisCA
http://www.google.com.eg/imgres?imgurl=http://www.gehealthcare.com/usen/ultrasound/images/cme_scrotal5_500.jpg&imgrefurl=http://www.gehealthcare.com/usen/ultrasound/products/cme_scrotal.html&usg=__pRNzx5ouiF10cwNwsoFkjfJSRXA=&h=500&w=500&sz=36&hl=en&start=3&sig2=ks6xO2TYTwxfQlNMvO1feQ&itbs=1&tbnid=OE4rpucS1ksjsM:&tbnh=130&tbnw=130&prev=/images%3Fq%3Dscrotal%2Bultrasound%26hl%3Den%26gbv%3D2%26tbs%3Disch:1&ei=HV8STNq1HdCg4QbzxKisCA
Sonographically the acute epididymitis usually shows enlargement of the epididymal head with decreased echogenicity secondary to edema. A reactive hydrocele may be present. Color Doppler findings include an increased amount of flow in and around the epididymis. If an abscess has formed, complex cystic areas may be identified in the epididymis.
http://www.google.com.eg/imgres?imgurl=http://www.gehealthcare.com/usen/ultrasound/images/cme_scrotal5_500.jpg&imgrefurl=http://www.gehealthcare.com/usen/ultrasound/products/cme_scrotal.html&usg=__pRNzx5ouiF10cwNwsoFkjfJSRXA=&h=500&w=500&sz=36&hl=en&start=3&sig2=ks6xO2TYTwxfQlNMvO1feQ&itbs=1&tbnid=OE4rpucS1ksjsM:&tbnh=130&tbnw=130&prev=/images%3Fq%3Dscrotal%2Bultrasound%26hl%3Den%26gbv%3D2%26tbs%3Disch:1&ei=HV8STNq1HdCg4QbzxKisCA
http://www.google.com.eg/imgres?imgurl=http://www.gehealthcare.com/usen/ultrasound/images/cme_scrotal5_500.jpg&imgrefurl=http://www.gehealthcare.com/usen/ultrasound/products/cme_scrotal.html&usg=__pRNzx5ouiF10cwNwsoFkjfJSRXA=&h=500&w=500&sz=36&hl=en&start=3&sig2=ks6xO2TYTwxfQlNMvO1feQ&itbs=1&tbnid=OE4rpucS1ksjsM:&tbnh=130&tbnw=130&prev=/images%3Fq%3Dscrotal%2Bultrasound%26hl%3Den%26gbv%3D2%26tbs%3Disch:1&ei=HV8STNq1HdCg4QbzxKisCA

 The normal testes should appear as small homogeneous ovoid structures with an echogenicity texture similar to the thyroid. The echogenic mediastinal stripe may be seen to flow through the mid section of the testis. The Doppler settings for color flow should be set for low volume, low velocity flow to optimize visualization of the small testicular arteries.
The normal testes should appear as small homogeneous ovoid structures with an echogenicity texture similar to the thyroid. The echogenic mediastinal stripe may be seen to flow through the mid section of the testis. The Doppler settings for color flow should be set for low volume, low velocity flow to optimize visualization of the small testicular arteries. 
 The scan can show the normal testes, epidydimis and scrotal contents.
The scan can show the normal testes, epidydimis and scrotal contents.It will show if there is a normal blood flow to both testes or if there is any inflammation or tumour. Varicocoeles, epidydimal cysts and hydrocoeles can also be detected.
Your scan will be performed by a radiologist who is a doctor specially trained in ultrasound scanning. You will be asked to lie on an examination bed and to remove your pants and trousers. You will be covered so only the scrotum is exposed. Lubricant gel is applied to the scrotum and a small probe is applied to the area. This produces sound waves which convert into an image of the testicles on the screen. The investigation does not hurt and will take approximately 10 minutes to perform.
http://www.google.com.eg/imgres?imgurl=http://www.andrologysolutions.co.uk/wp-content/uploads/2007/11/ultrasound-scrotum.jpg&imgrefurl=http://www.andrologysolutions.co.uk/%3Fpage_id%3D51&usg=__TNyi6ovZ-94zT6B5jiKxG5aI5-o=&h=298&w=400&sz=47&hl=en&start=1&sig2=fLkpabpmY0xQiGUae-j4Ew&itbs=1&tbnid=1Ng31CJ4iNNIpM:&tbnh=92&tbnw=124&prev=/images%3Fq%3Dscrotal%2Bultrasound%26hl%3Den%26gbv%3D2%26tbs%3Disch:1&ei=f1wSTJ68LJSS4ga0qpStCA
Subscribe to:
Comments (Atom)